

While the use of LABA/ICS is no longer encouraged in COPD 4, if patients with COPD have concomitant asthma, the use of ICS is mandatory 4.Īlthough the proportion of frequent exacerbators in the COPD population is generally less than 30%, and the proportion of eosinophilic exacerbators even lower (~10%) 16, 17, 18, 19, 20, 21, 22, 23, observational studies show that ICS-containing pharmacotherapy is prescribed in around 50–80% of patients with COPD 20, 22, 24, 25, 26, 27. In patients with blood eosinophils ≥100 cells/μl who continue to have exacerbations despite LAMA/LABA therapy, treatment can be escalated to triple therapy, after careful consideration of the expected benefits vs. Hence, the 2023 GOLD strategy report includes a practical recommendation for initial treatment with ICS (as LAMA/LABA/ICS triple therapy) in patients with frequent or severe exacerbations (≥2 moderate exacerbations per year, or ≥1 exacerbation requiring hospitalisation) and a blood eosinophil count ≥300 cells/μl 4. These changes occurred concurrently with an evolving understanding of the relatively narrow, phenotype-specific benefits of ICS use in COPD 14, 15. Since 2007, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy report has shifted its pharmacotherapy focus from a spirometry-based approach relying on the assessment of forced expiratory volume in 1 s (FEV 1 GOLD stages 1–4, GOLD 2007) to an exacerbation and symptom-based algorithm (GOLD grades A–D, GOLD 2011 to 2022 GOLD grades A/B/E, GOLD 2023) (Fig.
#Trelogy ics laba lama skin#
There is also evidence to suggest that long-term ICS use is associated with systemic adverse effects such as reduced bone mineral density (osteopenia), osteoporosis, fractures, diabetes, skin thinning and bruising, as well as ocular adverse effects such as cataract formation and glaucoma 8, 9, 10, 11. single or dual long-acting bronchodilator therapy, as well as a higher risk of oropharyngeal candidiasis, mycobacterial infections and upper respiratory tract infections 7, 8. ICS-containing regimens are associated with a higher risk of pneumonia vs.
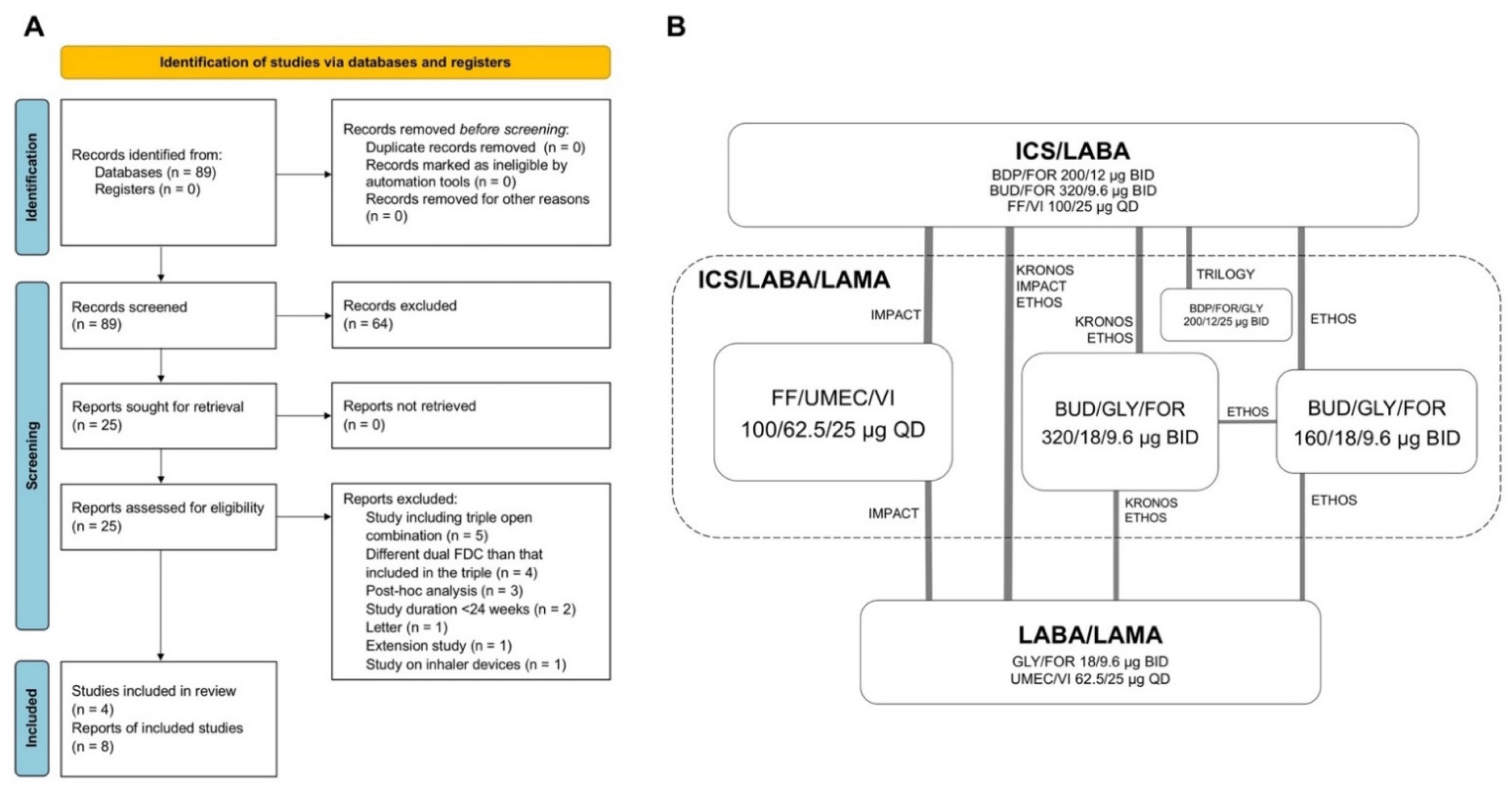
The major clinical benefit of ICS in COPD is a ~25% reduction in exacerbations in frequent or severe exacerbators, with no significant benefits in terms of lung function or mortality 5, 6. long-acting muscarinic antagonists (LAMAs) and long-acting β 2-agonists (LABAs), which in combination represent the mainstay of treatment for chronic obstructive pulmonary disease (COPD) 2, 3, 4.Īlthough ICS are effective in some patients with COPD, they are less effective in many others. In contrast, there is much debate about the role of ICS relative to long-acting inhaled bronchodilators, i.e. Inhaled corticosteroids (ICS) have long been the mainstay of asthma treatment, improving symptom control and reducing the risk of serious exacerbations 1. We also provide a practical guide to prescribing ICS, based on the latest global treatment guidelines, to help primary care providers identify patients for whom the benefits of ICS outweigh the risks. In this article, we review the benefits and risks of ICS use in COPD, drawing on evidence from RCTs and observational studies conducted in primary care. Prescription of ICS in patients not fulfilling guideline criteria puts patients at unnecessary risk of pneumonia and other long-term adverse events and also has cost implications, without any clear benefit in disease control. However, data from routine clinical practice indicate ICS overuse, with up to 50–80% of patients prescribed ICS. This reinforces guideline recommendations that ICS-containing maintenance therapy should be reserved for patients with frequent or severe exacerbations and high blood eosinophils (~10% of the COPD population), or those with concomitant asthma. Observational evidence from routine clinical practice demonstrates that dual bronchodilation is associated with better clinical outcomes than triple therapy in a broad population of patients with COPD and infrequent exacerbations. However, the suggestion of a mortality benefit associated with ICS in these trials has since been rejected by the European Medicines Agency and US Food and Drug Administration. Recent randomised controlled trials (RCTs) conducted in patients with COPD and frequent or severe exacerbations demonstrated a significant reduction (~25%) in exacerbations with ICS in combination with dual bronchodilator therapy (triple therapy). Inhaled corticosteroids (ICS) are the mainstay of treatment for asthma, but their role in chronic obstructive pulmonary disease (COPD) is debated.


 0 kommentar(er)
0 kommentar(er)
